
Esophageal cancer is one of the more aggressive malignancies we encounter. As the 17th most common cancer diagnosis in the United States, it is relatively rare. Despite this rarity, it is the sixth leading cause of cancer-related death. The overall survival for esophageal cancer, which we define as a patient’s chances of being alive five years after diagnosis, is only about 20%. As with all cancers, early detection is the best way to improve survival. Unfortunately, the options to screen for esophageal cancer are limited to those with Barrett’s esophagus. You should talk to your primary care provider or gastroenterologist about screening for esophageal cancer if you have more than one of the following risk factors: Barrett’s esophagus, hiatal hernia, age >/= 50, chronic GERD, Caucasian, central obesity and cigarette smoking.
Once a patient is diagnosed with esophageal cancer, the next step is to assess the stage of the cancer with a variety of imaging tests and procedures, as the stage will dictate the type of treatment. Stage 4 disease, with cancer spread to distant sites, is only treated with chemotherapy and radiation. Similarly, cancer in the upper third of the esophagus, which cannot be resected, is also treated with chemoradation. For all other stage cancers, treatment paradigms that include surgical resection offer the greatest survival advantage and chance of a cure. The surgical resection is typically preceded by chemotherapy or chemoradiotherapy. In the last year, a study was published comparing a newer chemotherapy regimen, “FLOT,” to the traditional chemoradiotherapy, “CROSS,” followed by surgery. This study showed a 5-year survival of the FLOT + surgery patients to be approximately 50%, while the survival in the CROSS + surgery arm was only 40%. This is quickly becoming the standard of care for many esophageal cancers.
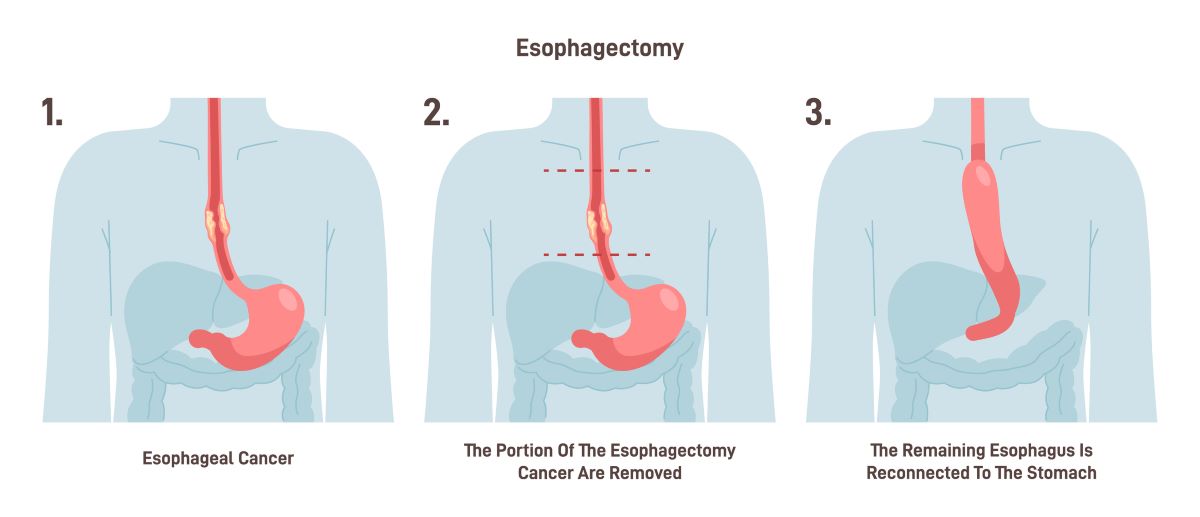
Resection of the esophagus has been the mainstay of surgical treatment for esophageal cancer since the early 20th century. In order to remove the cancer with adequate margins and then restore the patient’s ability to eat, the top of the stomach must be removed along with the involved esophagus. The remaining stomach is fashioned into a tubular “neo-esophagus” and sewn to the cut end of the esophagus either in the right chest or the neck. This is a complicated procedure to conceptualize and it is best to look at the figure below.
There are advantages and disadvantages to these choices and the superiority of one vs. the other is a topic of much discussion and debate. What isn’t up for debate is the benefit to the patient of performing the surgery via minimally invasive techniques. At Northside Hospital, we perform the surgery using the DaVinci Surgical Robot, which provides enhanced visualization and precision to rival or even surpass the surgeon's own vision and dexterity. More importantly, the surgery is less painful, allowing patients to return to normal activities sooner without compromising the removal of all of the cancer.
We have an excellent multidisciplinary team which leverages the vast resources of the Northside Health System in the areas of medical oncology, radiations oncology, radiology, pathology, thoracic surgery, nursing, genetics and research to create an individualized treatment for each and every patient. The surgical and postoperative care at Northside Hospital is second to none, which confers upon our patients the greatest chance to beat esophageal cancer with the lowest amount of morbidity.
Learn more about esophageal cancer treatment at Northside Hospital Cancer Institute.

